By David M. Briscoe, MD, ASCI, Transplant Research Program Director
At Boston Children’s Hospital (BCH), our ultimate goal is to ensure long-term graft survival following solid organ transplantation. This goal is achieved through the use of innovative new surgical techniques and new immunosuppressive medications that preserve organ function while allowing children to grow and develop as healthy adolescents and adults following transplantation. The Pediatric Transplant Center is home to world-class transplant teams who perform cutting-edge clinical trials to evaluate the effectiveness of new treatments and approaches to care.
To maximize our potential to accelerate discovery and ultimately to improve care, the Department of Medicine at BCH launched a Transplant Research Program. The focus of the Program is to perform basic research to further understand the molecular basis for chronic allograft rejection in children, the leading cause of graft failure following transplantation. Members of the Transplant Research Program have opportunities to interact with clinical programs, both locally and nationally, which allow the development of candidate biomarkers as a new tool to monitor for early signs of chronic rejection, before it’s too late to treat. Faculty within the Program are also assessing new avenues of research that challenge existing paradigms. Some have discovered roles for new cells and molecules that have potential to change our approaches to therapy, and they include the following:
- Dr. Soumitro Pal is uncovering novel signaling mechanisms underlying the cause of the increased risk of cancer in transplant recipients (Basu et al. Cancer Letters 2012). His research focuses on how targeted therapies can prevent post-transplantation cancer, and they have given us clues into molecules that may be useful as monitors of early pre-cancer events so that preventative therapy can be initiated.
- Dr. Kevin Daly’s studies received high-profile attention at the World Transplant Congress (July 2014) as he has identified a biomarker that predicts the development of chronic rejection at least four years before it occurs in heart transplant recipients. He discussed the impact of his studies in the Spring 2014 edition of the Transplant Talk newsletter.
- Dr. Gary Visner has been studying novel approaches for prolonging lung transplant survival. This work has recently identified two agents that prolonged lung allograft survival in the mouse lung transplant model. These agents reduced early injury and rejection, but more importantly, provided longer survival and reduced the development of transplant mediated fibrosis. In addition, they show promise as potential therapies for transplant patients (Liu et al Am J Respir Cell Mol Biol. 2014, Bizargity et al Transplantation 2012).
- Dr. Paolo Fiorina has been studying innovative ways to treat diabetes using immunosuppression, and his research led to the discovery of a new molecule and compound that has high potential for use as a treatment following transplantation (Vergani et al. Circulation 2013). Furthermore, his studies on this molecule have potential to lead to a biomarker assay that can predict chronic rejection.
- Drs. Natasha Frank and Markus Frank identified a stem cell pool that can be harvested from the eye and can be used to grow cornea in vivo. This is one of the first examples of constructing a fully functional human tissue from a molecularly defined adult human stem cell. Application of this research technology has the potential to lead to novel stem cell-based approaches to corneal transplantation and hopefully to other tissues and organs in the future (Ksander et al. Nature 2014).

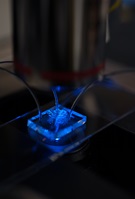
- A member of my own research laboratory collaborated with Dr. Irimia, a bioengineer at the Massachusetts General Hospital, to identify how inflammatory cells crawl in and out of an allograft. A new technique, called microfluidics, allowed us to visualize individual cells as they start to move. We found that these rejection-causing cells move in a stop-and-start pattern, at different speeds, and can even reverse direction away from a potent attractive stimulus (Boneschansker et al. Nature Communications 2014). Further understanding of this reverse migration process where cells move away from a stimulus could lead to the development of new anti-rejection therapeutics. Other work in collaboration with Dr. Michael Klagsbrun of the Vascular Biology Program received an award at the World Transplant Congress (July 2014) and identified a new family of molecules that enhance the resolution of inflammation.
Overall, we are making great strides in our efforts to enhance discovery at BCH. Due to space limitations, I’ve only given a few highlights to describe our ongoing research progress; many other innovative studies are ongoing. I encourage you to visit our website to see the breadth of transplant research that is here at BCH. It’s a very exciting time, as the current era allows discoveries to be quickly translated into therapies for patients and it is inevitable that in the not-so-distant future, we will develop new medications and use new monitoring assays and biomarkers to predict events before they happen. We’re constantly encouraged at how excellence in patient care is enhanced through basic research discoveries.

Learn more about how you can help support our efforts by contacting Dr. David Briscoe, David.Briscoe@childrens.harvard.edu or Melanie Torosyan, Senior Major Gifts Officer at Boston Children’s Hospital Trust, 617-355-4102, Melanie.Torosyan@chtrust.org.
